The incidence of ectopic pregnancy is about 2%. The mortality connected with ectopic pregnancies in the united states is about 0.50 deaths per 100,000 live births (Creanga AA et al., 2011). This shows exactly how important it is to set the proper diagnosis in time.
Risk Factors
- previous ectopic pregnancy
- previous chlamydia trachomatis infection
- history of infertility
- treatment with IVF for tubal infertility
- previous adnexal surgery including sterilization
- previous or current use of IUDs
- smoking
- poor education and poor occupation (Li C et al., 2015)
- endometriosis (Yong, PJ et al., 2020).




Approximately half of all women with an ectopic pregnancy present without known risk factors.
(Creanga AA et al., 2011).
Diagnosing a Tubal Ectopic
#1 – The Blob Sign
Tubal ectopic pregnancies should be identified by visualising an adnexal mass that is separate from the ovary (Elson CJ et al., 2016). The presence of this inhomogeneous mass which is clearly not a part of the ipsilateral ovary or of the uterus is called the blob sign (Nadim B. et al, 2017).

#2 – The Bagel Sign
The empty gestational sac and the decidualized tubal epithelium around it create an image similar to a bagel, or bagel sign (Nadim B. et al, 2017).

#3 – Adnexal Mass Mobility
The ovary and ipsilateral tube are anatomically very close to one-another.


Thus, when a tubal ectopic is suspected and a para-ovarian mass is seen consider testing for adnexal mass mobility:
- Place the endovaginal transducer as a wedge between the para-ovarian mass and the ovary.
- Apply gentle pressure either with your free hand transabdominally, or with the endovaginal transducer itself.
This maneuver may demonstrate obvious movement of each structure in different directions, aiding in the differential between ovarian cyst and tubal ectopic.
Be cautious however:
- Adhesions may prevent separate movement of the tube and the ipsilateral ovary.
- Mobile para-ovarian mass is not always an ectopic; do not forget that parovarian cysts (Morgagni’s hydatid cysts) are also very mobile.
#4 – Color Doppler
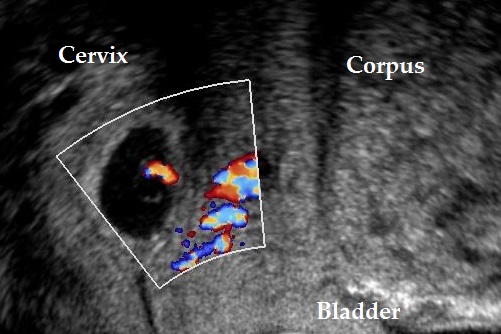
Color doppler signals may help in the diagnosis of the tubal ectopic pregnancy as they are clearly separated from ovarian tissue (Alkatout, I et al., 2013).
Keep in mind that both the corpus luteum cyst and the tubal ectopic may have similar appearance and both demonstrate ring-like color flow patterns (Fukami, T et al., 2006).

Tiny tubal ectopic. 
Color doppler of the same ectopic. 
Color doppler of a corpus luteum graviditatis.
#5 – 3D Ultrasound
3D-ultrasound has not yet been proven to actually improve the diagnostic accuracy in tubal ectopic pregnancy (Infante, F et al., 2018). Still the power to create custom imaging planes may facilitate the diagnostic procedure.

You might also find interesting other articles on ectopic pregnancy:
Bibliography
- Creanga AA, Shapiro-Mendoza CK, Bish CL, Zane S, Berg CJ, Callaghan WM. Trends in ectopic pregnancy mortality in the United States: 1980-2007. Obstet Gynecol. 2011 Apr;117(4):837-43. doi: 10.1097/AOG.0b013e3182113c10.
- Li C, Zhao WH, Zhu Q, Cao SJ, Ping H, Xi X, Qin GJ, Yan MX, Zhang D, Qiu J, et al. Risk factors for ectopic pregnancy: a multi-center case–control study. BMC Pregnancy childbirth. 2015;15:187. doi: 10.1186/s12884-015-0613-1.
- Elson CJ, Salim R, Potdar N, Chetty M, Ross JA, Kirk EJ on behalf of the Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy. BJOG 2016;. 123:e15–e55.
- Nadim, B., Infante, F., Lu, C., Sathasivam, N. and Condous, G. (2017), The morphological ultrasound types known as ‘blob’ and ‘bagel’ signs should be reclassified from probable to definite ectopic pregnancy. Ultrasound Obstet Gynecol. Accepted Author Manuscript. doi:10.1002/uog.17435
- Blaivas, M., & Lyon, M. (2005). Reliability of adnexal mass mobility in distinguishing possible ectopic pregnancy from corpus luteum cysts. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 24(5), 599–605. https://doi.org/10.7863/jum.2005.24.5.599
- Yong, P. J., Matwani, S., Brace, C., Quaiattini, A., Bedaiwy, M. A., Albert, A., & Allaire, C. (2020). Endometriosis and Ectopic Pregnancy: A Meta-analysis. Journal of minimally invasive gynecology, 27(2), 352–361.e2. https://doi.org/10.1016/j.jmig.2019.09.778
- Alkatout, I., Honemeyer, U., Strauss, A., Tinelli, A., Malvasi, A., Jonat, W., Mettler, L., & Schollmeyer, T. (2013). Clinical diagnosis and treatment of ectopic pregnancy. Obstetrical & gynecological survey, 68(8), 571–581. https://doi.org/10.1097/OGX.0b013e31829cdbeb
- Fukami, T., Emoto, M., Tamura, R., & Kawarabayashi, T. (2006). Sonographic findings of transvaginal color Doppler ultrasound in ectopic pregnancy. Journal of medical ultrasonics (2001), 33(1), 37–42. https://doi.org/10.1007/s10396-005-0064-9
- Infante, F., Espada Vaquero, M., Bignardi, T., Lu, C., Testa, A. C., Fauchon, D., Epstein, E., Leone, F., Van den Bosch, T., Martins, W. P., & Condous, G. (2018). Prediction of Tubal Ectopic Pregnancy Using Offline Analysis of 3-Dimensional Transvaginal Ultrasonographic Data Sets: An Interobserver and Diagnostic Accuracy Study. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 37(6), 1467–1472. https://doi.org/10.1002/jum.14489